What is Amniocentesis?
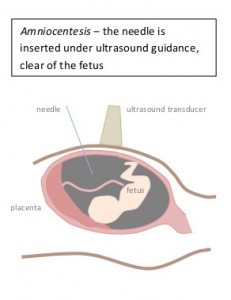
Amniocentesis is a procedure in which a fine needle is passed through the maternal abdomen and uterine wall to collect some amniotic fluid from around the fetus. Cells within the amniotic fluid have the same genetic material as the fetus and can therefore be tested for specific chromosomal and genetic conditions.
Who is offered Amniocentesis?
Amniocentesis is offered to patients who are at increased chance of having a child with a chromosomal difference.
This may include:
- Increased chance screening results on NIPT or first/second trimester screening
- Increased nuchal translucency or other ultrasound findings
- Family history of a chromosomal or genetic condition
- Individuals/couples are known carriers of a genetic condition
- Advanced maternal age (maternal age above 37)
How is it performed?
An ultrasound examination is first performed to a) confirm the dates, b) to assess the position of the placenta, and c) assess the baby for ultrasound signs related to genetic/chromosomal differences. The test is performed at the ultrasound clinic by an Obstetrician Gynaecologist Sonologist (specialist ultrasound doctor).
The skin of the lower abdominal wall is cleansed with an antiseptic alcohol-based solution. The amniocentesis needle is then guided into the amniotic fluid by tracking its course on the ultrasound screen. It takes about 30 seconds to draw up the 20 mL of straw-coloured fluid required for analysis. The volume of fluid aspirated is about 1/6th of that present around the fetus and this is naturally replaced over the next 24 hours.
When is it performed?
An amniocentesis is usually performed any time after 15 weeks and 4 days of gestation.
What preparation is required prior to the procedure?
You will need to bring a
- Referral from your doctor
- Reports for the pregnancy (if performed elsewhere)
- Your blood group card
A moderate amount of fluid in the bladder is preferable. This can help make the uterus more accessible for the needle test.
How is the amniotic fluid analysed?
The specimen is sent to a laboratory to be processed.
The type of testing performed by the laboratory will depend on the indication for the test. Our genetic counsellors will discuss this further with you.
What is to be expected after the test?
It is advisable for someone to take you home after the test and that you rest for the remainder of the day. This does not mean you should confine yourself to bed but rather you should just rest at home and avoid any strenuous activity including lifting any heavy weights.
Most patients experience a short duration of mild crampy period-like pains. This is most likely to occur after the local anaesthetic wears off, i.e., within the first half hour after the test. You may wish to take paracetamol or panadol.
It is not unusual for some patients to experience slight vaginal blood spotting after the test.
If the pains worsens or spotting progresses to fresh red bleeding, then contact your doctor.
What are the risks of the test?
There is a 1 in 1000 (0.1%) risk of miscarriage with the test. This is usually related to infection introduced at the time of the procedure. Antiseptic precautions are taken to minimise this risk.
Warning signs of miscarriage include strong regular period like pains with fresh red bleeding. The time when miscarriage is most likely to occur is the first 24-48 hours after the test. Contact your doctor should this occur.
How long before I know the results?
Results vary depending on the testing ordered. Most results take around two weeks (10 business days) to come back. Our genetic counselling team will contact you or your doctor by phone with the result. Your doctor will also receive a copy of the report from the laboratory.